Diabetes: two conditions, one name.
Diabetes, a word derived from ancient Greek, originally described the passing of large quantities of urine – something today we would consider uncontrolled diabetes. The word came into medical usage when the differences between Types 1 and 2 Diabetes were not appreciated. And therein lies a problem; a problem because although Type-1 and Type-2 Diabetes sound similar, they are very different conditions.
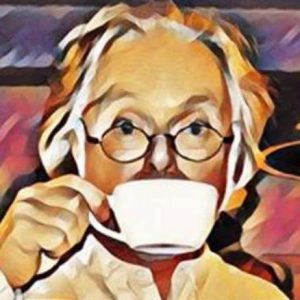
People with Type-1 Diabetes typically ‘present’ in childhood or as younger adults. Type-1 is caused by damage to cells within the pancreas, particularly those that make insulin (beta-cells). Type-1 is an auto-immune condition, a condition where the body attacks its own cells with antibodies. What causes the antibodies to attack is not known for sure but viral infections may be a trigger. The result is that little or no insulin gets produced. One of insulin’s jobs is to bring blood sugar (glucose) levels down. So, in Type-1 glucose levels go up and eventually glucose appears in the urine too (glycosuria). Without insulin, the body’s cells become starved of glucose and malfunction. Indeed, before the introduction of insulin injections, untreated Type-1 Diabetes was almost always fatal. Type-1 is now treated with insulin injections. It is a form of hormone replacement therapy; the hormone being insulin. Typically, someone with Type-1 has to regularly inject themselves with insulin to control the surges in blood glucose after meals and to help glucose get into cells to keep them functioning.
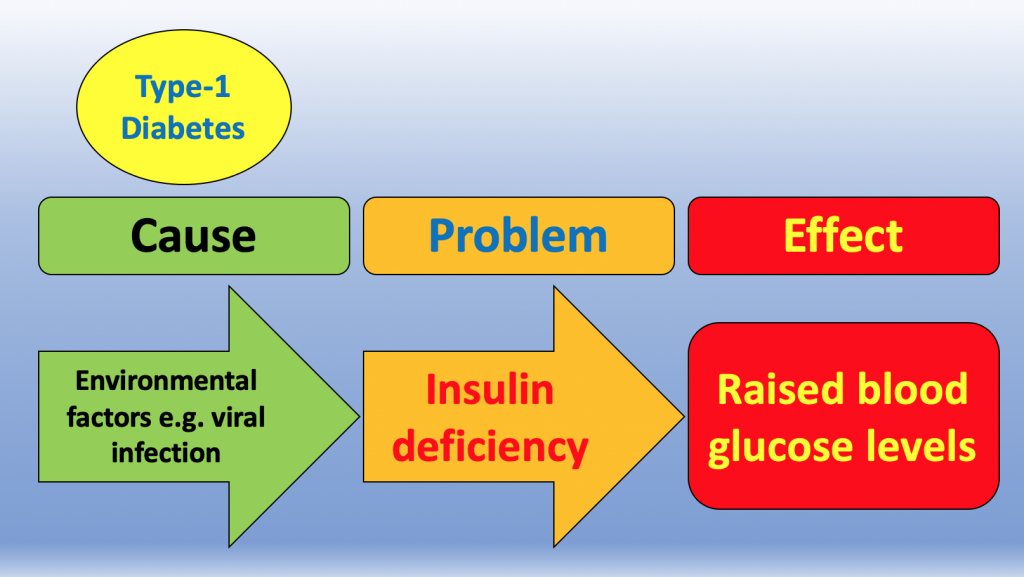
Type-2 Diabetes is different; almost the opposite in fact. Early on, there is plenty of insulin – typically there is too much insulin around. The problem is that the body has stopped responding to it. The technical term for this is insulin resistance. Indeed Insulin Resistance is the principal abnormality driving Type-2 Diabetes. The cause of Type-2 is not down to a virus. Rather, it is usually the consequence of years of eating the wrong foods – foods that cause large blood glucose surges following meals: too much glucose and for too long. So, Type-1 requires insulin replacement therapy and Type-2 requires dietary change or, more commonly, drugs.
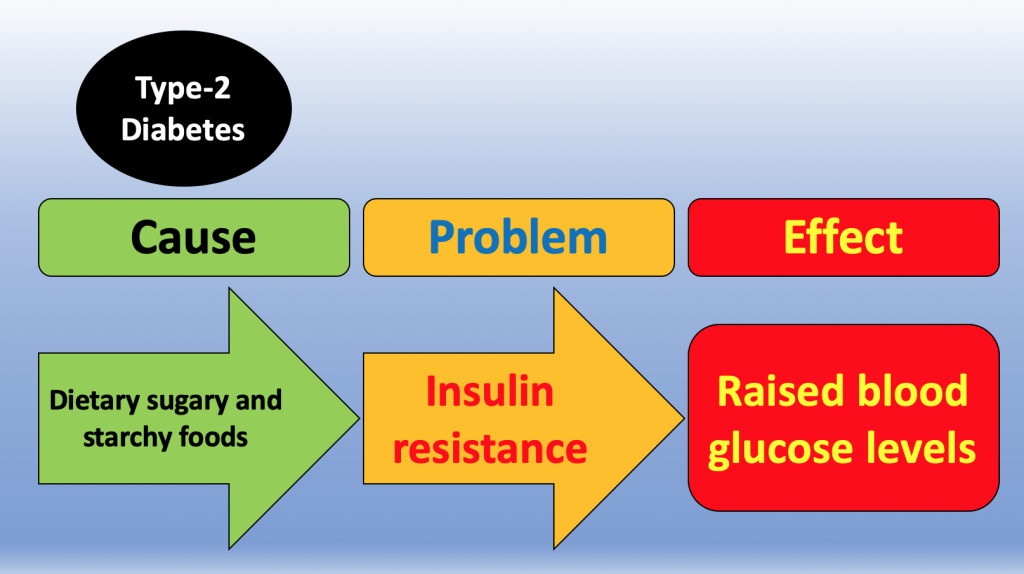
But here is a weird thing, something not appreciated by many with diabetes. Most people with Type-1 will eventually get Type-2 as well. It’s even got a name – double diabetes. Because of their sugary and starchy dietary choices, they can get insulin resistance on top. Typically, they will notice their insulin requirements going up; more insulin is needed to overcome the insulin resistance. They may also have found that weight goes up too. And, sadly, they will then be at risk of the many complications so frequently seen in Type-2 Diabetes. You see, if someone with Type-1 consistently avoids consuming a lot of sugary and starchy foods they rarely develop insulin resistance. All those medical checks they get (vision, nerve function, circulation, cholesterol, etc.) are in large part to do with insulin resistance; features of Type-2 Diabetes in other words.
And here is another weird thing. Many people with Type-2 will eventually become unable to make enough insulin. It’s called beta-cell failure and seems to be caused by running blood glucose levels too high for too long. There appears to be something ‘toxic’ about having too much glucose around. Typically, beta-cell failure comes on after years of escalating medical treatment with anti-diabetic drugs. They will have had their medication stepped up repeatedly over the years trying ever harder to keep the lid on their diet-driven surging glucose levels. Yup, their medication is there to treat their food choices. But when beta-cell failure develops the only option is to add insulin injections to all those drugs. They too now need insulin replacement therapy.
So, what to do?
Firstly, if you have Type-1 and do not want to get Type-2 on top (double-diabetes), consider doing a little research into low-carb dining. The aim would be to cut your insulin requirements and avoid developing insulin resistance. Even Type-1s mainly need insulin injections to cover their dietary carb choices. Diet change must be done very carefully and with the help of your health professionals. Why? because your insulin requirements will go down. You do not want to take the considerable risks of hypoglycaemic attacks.
Secondly, if you have Type-2 and do not want to end up needing insulin, consider doing a little research into low-carb dining. The aim would be, over time, to reduce your insulin resistance. Again, diet change must be done very carefully, and with the help of your health professionals. Why? because your medication requirements may go down. You do not want to take the considerable risks of hypoglycaemic attacks.
As a wise doctor once said, “It’s all about the insulin…”